Foot fungus: Types and treatments
What is Foot Fungus?
Foot fungus refers to a group of fungal infections that affect the skin, toenails, or spaces between the toes. These infections develop when dermatophytes (fungi that feed on keratin) or yeast overgrow in warm, moist environments such as sweaty socks, tight shoes, public showers, and locker rooms. Foot infection can begin with mild itching or peeling between the toes but may progress to severe pain, cracked skin, or thickened, discoloured toenails if untreated.
Common foot fungal infection types include athlete’s foot (tinea pedis), toenail fungus (onychomycosis), moccasin-type tinea, vesicular infections, and yeast infections. Symptoms may vary but often involve redness, burning, scaling, foul odour, or brittle nails.
People with diabetes, weakened immunity, or poor foot hygiene are at higher risk of developing these infections. For diabetic patients, even minor foot fungal infections can lead to serious complications like ulcers or cellulitis if not treated promptly. Therefore, maintaining proper foot hygiene, wearing breathable shoes, and keeping feet dry are essential preventive measures. Diabetic patients should seek regular foot therapy for diabetes to reduce the risk of infections. Early diagnosis and timely foot fungal infection treatment ensure faster recovery and prevent recurrence.
Types of Foot Fungal Infections
There are several foot fungal infection types that affect different areas of the feet:
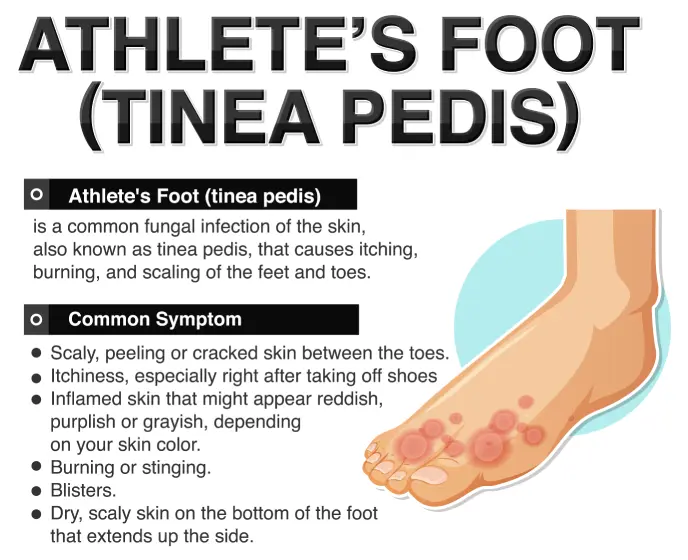
Athlete’s Foot (Tinea Pedis)
- The most common foot fungal infection type especially among athletes or those wearing closed shoes for long hours.
- Caused by dermatophyte fungi that thrive in moist environments.
- Symptoms include itching, burning, peeling skin, and redness, especially between toes.
Toenail Fungus (Onychomycosis)
- Affects toenails, making them thickened, discoloured (yellow, brown, or white), brittle, or crumbly.
- Without prompt foot fungal infection treatment, it can lead to pain and difficulty wearing shoes.
Moccasin-Type Tinea
- Affects the soles and sides of the feet, resembling dry, scaly skin or eczema.
- Often chronic and requires persistent fungal infection treatment on the skin.
Vesicular Infection
- Less common, characterised by fluid-filled blisters, usually on the sole.
- May cause discomfort while walking.
Yeast Infections
- Candida infections can occur, especially in diabetic patients, causing redness, soreness, and white patches.
Symptoms of Fungal Infection in Feet
Recognising the symptoms of fungal infection in feet early is crucial for prompt treatment and preventing complications. The most common signs include persistent itching or burning sensations, especially between the toes, which is often seen in athlete’s foot (tinea pedis). The affected skin may appear red, scaly, or cracked, leading to discomfort while walking.
In some cases, foot fungal infections cause peeling skin, blisters, or ulcers, particularly if the infection is severe or left untreated. Toenail fungus (onychomycosis) presents differently, causing nails to become thickened, discoloured (yellow, brown, or white), brittle, crumbly, or even distorted in shape. A foul odour from the feet or nails may accompany these symptoms due to fungal overgrowth.
People with diabetes must be extra cautious, as minor foot infection symptoms can progress into serious issues like cellulitis or diabetic foot ulcers. Other signs of foot fungal infection include fluid-filled blisters (vesicular type), pain, or a burning sensation on the sole in moccasin-type tinea.
If these fungal infection symptoms persist despite home care, consult a doctor for proper foot fungal infection treatment. Early medical intervention ensures faster healing, prevents spread to other body parts, and reduces the risk of chronic or recurrent infections
Recognising fungal infection symptoms early ensures faster recovery. Common signs include:
- Persistent itching or burning sensation.
- Peeling, cracked, or scaly skin.
- Redness and inflammation.
- Thickened, discoloured, or brittle toenails.
- Foul odour from feet or nails.
- Fluid-filled blisters in vesicular infections.
- Pain or discomfort while walking
If these fungal infection symptoms persist despite home remedies, consult a doctor for appropriate foot fungal infection treatment.
Treatment Options for Foot Fungal Infections
Effective fungal infection treatment on the skin depends on the type and severity. Common foot fungal infection treatments include:
Topical Antifungal Medications
- Creams, sprays, or powders containing clotrimazole, miconazole, or terbinafine.
- Ideal for athlete’s foot and mild skin infections.
- Apply as per prescription for at least 2-4 weeks, even if symptoms resolve early.
Oral Antifungal Medications
- For severe or stubborn foot fungal infections, especially toenail fungus.
- Common medications: terbinafine or itraconazole.
- Require a doctor’s prescription and regular monitoring for side effects.
Antifungal Nail Lacquers
- Special medicated nail paints to treat toenail fungus.
- Used daily or weekly, depending on formulation.
Home Remedies (Supportive Care)
- Keeping feet clean and dry.
- Using antifungal foot powders.
- Wearing breathable cotton socks and moisture-wicking shoes.
- Soaking feet in warm saltwater or diluted vinegar solutions (supports treatment but does not replace medical therapy)
Foot Therapy for Diabetes
People with diabetes are prone to severe foot infections. They must:
- Inspect feet daily for cracks, ulcers, or fungal changes.
- Seek podiatry care for routine nail trimming and callus removal.
- Use prescribed antifungal treatments under medical supervision.
- Maintain controlled blood sugar to promote healing
Laser Treatment
- An emerging option for toenail fungus, where targeted laser destroys fungal organisms.
- Requires multiple sessions and may not be covered by insurance.
When to See a Doctor?
Consult a doctor if:
- Symptoms persist despite using OTC antifungal creams for two weeks.
- Nails are thickened, painful, or discoloured.
- There are signs of bacterial infection (swelling, pus, fever).
- You have diabetes with any foot fungal infection symptoms.
- Blisters rupture or ulcers develop
Early medical intervention prevents complications and ensures proper foot fungal infection treatment.
Conclusion
Foot fungal infections are common but treatable. Understanding foot fungal infection types, from athlete’s foot to toenail fungus, helps in early identification. Effective fungal infection treatment on skin, including topical or oral antifungals, good foot hygiene, and foot therapy for diabetes, ensures faster healing and prevents recurrences. If symptoms persist, consult your dermatologist or podiatrist for tailored foot fungal infection treatment to maintain healthy, comfortable feet.
FAQs
What are the common signs of a foot fungal infection?
The most typical fungal infection symptoms include persistent itching, burning sensations, peeling or cracked skin, redness between the toes, and foul odour. In toenail infections, you may notice thickened, brittle, or discoloured nails. Identifying these fungal infection symptoms early can help start timely foot fungal infection treatment and prevent complications.
How do I know which type of foot fungus I have?
There are several foot fungal infections types, each affecting different areas. Athlete’s foot usually appears between the toes, moccasin-type tinea affects the soles, and toenail fungus causes nail discolouration and thickening. A healthcare provider can examine your feet and recommend the appropriate fungal infection treatment for skin or nails based on your symptoms.
What is the most effective foot fungal infection treatment?
The best foot fungal infection treatment depends on the severity and type. Mild cases often respond to topical antifungal creams or powders. Persistent or nail-based infections may require oral antifungals or medicated nail lacquers. In some cases, laser therapy or prescription treatments are necessary. For lasting results, combine medication with proper foot hygiene and supportive care.
Can people with diabetes get fungal foot infections more easily?
Yes. People with diabetes are more prone to foot infections due to poor circulation and weakened immunity. Even minor fungal infections can escalate into serious complications. That is why foot therapy for diabetes is critical; regular checkups, early detection, and medically supervised care help in managing foot fungal infection types effectively and safely.
When should I see a doctor for a fungal infection on my foot?
If your fungal infection symptoms do not improve with over-the-counter products within two weeks, or if you notice blisters, ulcers, nail thickening, or signs of bacterial infection (e.g., swelling, pus, fever), consult a doctor immediately. Timely fungal infection treatment on skin and nails prevents recurrence and avoids further damage, especially for diabetic patients.


.jpg)

